From Despair to Hope: How Advocacy Saved Audrey’s Life

Audrey, a spirited 5-year-old from Spartanburg, South Carolina, embodies a story defined by perseverance, the power of love, and a mother’s relentless determination to uncover the truth behind her child’s mysterious symptoms.
When Audrey was three and a half, she began experiencing neck pain that came and went in short, excruciating bursts. “She would grab her neck and scream, ‘My neck, my neck!’” recalls her mother, Becky. “At first, we thought it was muscular. She had just started daycare and was getting sick often, so we thought it was related to that.” The pain would ease up for a while but it would inevitably return, worse than before. Months passed with the sporadic neck pain, then vomiting became another symptom. Becky and her husband, Brett, initially attributed this to Audrey’s history of severe reflux. They just hadn’t yet connected the dots.
As the symptoms persisted over the next year and a half, Becky grew more concerned. “I said to her doctor, ‘Something isn’t right. This has been going on way too long’,” Becky explains. The family’s pediatrician agreed and referred her to a neurosurgeon in Greenville, South Carolina. The doctor in Greenville suspected Audrey had a Chiari malformation, a structural defect in the cerebellum that can cause symptoms similar to what Audrey was experiencing. However, an MRI revealed a far more serious diagnosis: a tumor. “The very first image they took showed the mass,” Becky shares. “They spent two and a half more hours scanning her spine for other tumors, but fortunately, none were found.”
At this point, Becky knew she needed to get the best possible care for her daughter. “Our neurosurgeon was amazing—she encouraged me to seek a second opinion, reassuring me she wouldn’t be offended. As a mother herself, she understood my desire to find the best possible care for my child,” Becky recalls. “I did extensive research and found another highly regarded neurosurgeon in South Carolina. We needed answers quickly because the tumor, a low-grade glioma, was pressing into Audrey’s brain stem and cerebellum.”
The second neurosurgeon, however, painted a grim picture. “He told us there was a 100% chance Audrey would have deficits if surgery was performed. He said she wouldn’t be able to breathe on her own, she’d likely need a trach and a feeding tube, and it was unlikely he could remove the entire tumor. We were devastated. It was impossible to believe that this was our only option.”
Feeling helpless, Becky turned to social media, joining pediatric low-grade glioma groups on Facebook to ask other families about their experiences. The response was overwhelming. One particular doctor in Memphis, Tennessee, was recommended repeatedly. “One mom reached out and asked me for my phone number, which she then shared directly with this world-renowned pediatric neurosurgeon. An hour later, he called me—on a Saturday, while at his son’s lacrosse game—to talk to me about my daughter’s brain tumor! Who does that?!”
The doctor, affiliated with Le Bonheur Children’s Hospital and St. Jude’s Children’s Research Hospital, both in Memphis, offered the family hope. He believed he could remove Audrey’s tumor without leaving her impaired, thanks to a cutting-edge intraoperative MRI tractography (iMRI) machine, which would allow him and his surgical team to monitor and remove even the tiniest remnants of the tumor without damaging the surrounding brain tissue.
But Audrey would have to travel to Memphis for this procedure because no hospital in South Carolina offered this technology.
So while Becky and Brett were filled with hope, they faced a significant hurdle—Audrey’s insurance, Medicaid, would not cover her surgery out of state. Despite their efforts to petition the decision, they were told Medicaid’s policy only occasionally allows out-of-state coverage, and then only following a lengthy appeal process. The red tape was delaying critical care, and for Audrey, time was of the essence.
“It was devastating. We were running out of time, and the appeal process was taking too long,” Becky shares.
With insurance issues complicating the situation, Becky and Brett, along with their friends and family, launched a fundraising campaign to cover Audrey’s out-of-state surgery. A plan was then set for Audrey to be admitted to the Emergency Room at Le Bonheur Hospital where state of residence wouldn’t be a factor in her receiving medical treatment. Once admitted, she would be scheduled for surgery.
The operation was long—over 13 hours—but it was a success. “When the doctor called me from the operating room and said, ‘We got it all,’ it was the best moment of my life, even better than giving birth,” recalls Becky emotionally. “I couldn’t stop thanking him and his team. I mean it was a genuine miracle.”
Audrey spent one night in the ICU and just four more days in the hospital. Within three days of the surgery, she was walking and eating normally, following some right side post-operative weakness. Two days later she was discharged. “Every day just brought massive improvements,” Becky says.
Following the surgery, the St. Jude’s tumor board approved Audrey for follow-up treatment, and further classified her tumor as a juvenile pilocytic astrocytoma with a BRAFF mutation. This additional genetic classification is significant because if Audrey’s tumor were to ever return, targeted therapies could be used to treat it.
Today, Audrey is thriving. She’s in kindergarten, running, playing, and enjoying all the things a 5-year-old should. “The only sign of her surgery is a faint scar on the back of her head. You’d never know what she’s been through,” Becky shares. “She loves unicorns, swimming, mermaids, and playing dress-up—but she always wears shorts under her dresses so she can be ready to play and be rough and tumble!”
Reflecting on their journey, Becky emphasizes the importance of advocacy. “If I hadn’t pushed for that second and third opinion, I don’t think Audrey would be here today. Parents know when something isn’t right with their child. Keep advocating, keep pushing. Vague, undefined symptoms aren’t always nothing.”
Audrey’s experience highlights a critical issue in pediatric healthcare: the difficulties families face when seeking out-of-state treatment under Medicaid. Fortunately, recent legislative progress offers a glimmer of hope. The Accelerating Kids’ Access to Care Act [link to short article on AKACA and its current status], which aims to streamline Medicaid’s approval process for out-of-state pediatric specialty care, was recently passed by the House and now awaits a vote in the Senate. If enacted, this law could eliminate some of the obstacles that delayed Audrey’s care, allowing families to receive timely treatment without the burden of endless red tape.
For families facing a pediatric brain tumor diagnosis, Becky urges them to seek support. The Pediatric Brain Tumor Foundation offers invaluable resources and a community that understands the journey from diagnosis through treatment and beyond. If you or a family you know needs support, visit curethekids.org/support-for-families for a wealth of helpful information. If you would like to learn more about becoming an advocate with PBTF, visit curethekids.org/advocacy. You can also connect with our Patient Family Advocacy team by completing this brief form or emailing [email protected] anytime.
Related Stories

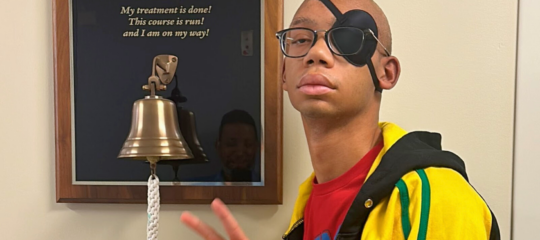
Patrick’s Recovery Through Laughter, Learning, and Sheer Determination

A Circle of Support: The Kaczmarski Family’s Journey from Receiving to Giving Back
Related Updates
Traveling for Brain Tumor Treatments: How to Plan for Out-of-State or International Care
Traveling for brain tumor treatment can be overwhelming, but with the right preparation and support, it can also be a journey filled with hope and resilience.
The Pediatric Brain Tumor Foundation welcomes Day One Biopharmaceuticals’ renowned Dr. Samuel C. Blackman to its Board of Directors