Summer 2023 Legislative Update: Childhood Cancer Bills We’re Tracking
Advancements in adult cancer treatments have shown time and again that no single group or person can end cancer. Federal agencies and the pharmaceutical industry must work with families, researchers, nonprofits, and patient advocates to remove barriers and find solutions.
Collaboration is at the heart of the White House’s reignited Cancer Moonshot initiative, which set goals to reduce cancer mortality by at least 50% over the next 25 years and improve the lives of cancer patients, survivors, their families, and caregivers. To realize this vision, the National Cancer Institute (NCI) released a National Cancer Plan this week that provides a road map for collaboration across the federal government and all parts of society.
NCI’s National Cancer Plan identifies eight goals that must be achieved to end cancer as we know it, strategies for each goal, and a call to action that reinforces the responsibility we all share.
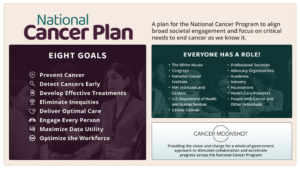
Infographic from nationalcancerplan.cancer.gov/about
In reviewing the full plan, we are encouraged by its more inclusive vision, emphasis on pediatric and rare cancer research, and strategies that align with our efforts to close gaps in pediatric brain tumor research, family support, and community engagement. Tissue donation, data sharing, precision medicine, health literacy, clinical trial expansion and access, eliminating inequities in healthcare, and strengthening diversity and inclusion in the cancer research workforce are just a few of the things we champion because they ultimately benefit kids with brain cancer.
Although the National Cancer Plan offers several steps in the right direction, it misses an opportunity to define pediatric-specific strategies in two important areas: early detection and cancer survivorship.
These overlooked opportunities underscore the fact that achieving the National Cancer Plan’s goals requires the perspectives and participation not only of government agencies and policymakers, but also patient families, advocacy organizations, healthcare providers, the commercial sector, and individuals.
The unique needs of pediatric patients, survivors and families must be heard and addressed. And they must be heard now. A recent report revealed more children in our country are diagnosed and dying from brain cancer than ever before, while incidence and mortality rates in adults are decreasing. Significant disparities in pediatric brain cancer incidence and mortality rates also exist across states, in part because of a lack of resources and funding and barriers that unnecessarily delay families’ access to care.
The Pediatric Brain Tumor Foundation is committed to leading the way toward a future without childhood cancer, but we can’t do it alone. A founding member of the Alliance for Childhood Cancer, we work with families to speak with one voice to Congress about the most urgent issues facing the childhood brain cancer community. And to address the significant disparities in resources and funding that exist in local communities, we’re spearheading a new initiative to get language and funding specific to childhood cancer and pediatric brain tumors included in every state cancer plan.
These initiatives are fueled by people just like you – pediatric brain cancer patients, survivors, parents, siblings, caregivers, and compassionate individuals who understand the burdens families face.
The time is now to be an advocate with the Pediatric Brain Tumor Foundation and work with us in your community to enact critical policy changes. Sign up for our upcoming advocacy webinar on April 19 or email the Pediatric Brain Tumor Foundation’s Director of Advocacy Mike Henry at [email protected] to learn how.